A study from Griffith University found a connection between nose-picking and an elevated risk of dementia.
Important bacterial species have a clearer road to the brain in situations when picking at your nose damages internal tissues, and the brain reacts to their presence in ways that are similar to symptoms of Alzheimer’s disease.
There are many limitations to this research, not the least of which is that the supporting research has thus far been conducted on mice rather than humans.
Nevertheless, the findings are definitely worth further study and may advance our comprehension of how Alzheimer’s disease develops, which is still largely unknown.
Researchers from Griffith University in Australia conducted experiments with the Chlamydia pneumoniae bacteria, which can infect people and result in pneumonia. Additionally, the bacteria has been found in the majority of human brains with late-onset dementia.
It was determined that the bacteria could ascend the olfactory nerve in mice (joining the nasal cavity and the brain). Additionally, nerve infections were worse when the nasal epithelium, the thin tissue that lines the roof of the nasal canal, was damaged.
As a result, the amyloid-beta protein, which is secreted in response to infections, was deposited in the mouse brains in greater amounts. People with Alzheimer’s disease have substantial amounts of plaques (or clumps) of this protein as well.
“We’re the first to show that Chlamydia pneumoniae can go directly up the nose and into the brain where it can set off pathologies that look like Alzheimer’s disease,” says neuroscientist James St John from Griffith University in Australia.
“We saw this happen in a mouse model, and the evidence is potentially scary for humans as well.”
The rapidity with which C. pneumoniae infected the central nervous systems of the mice—infection occurring within 24 to 72 hours—surprised the investigators. Bacteria and viruses may view the nose as a direct path to the brain, according to certain theories.
Even if it’s not known that amyloid-beta plaques cause Alzheimer’s disease or that the consequences would be the same in people, it’s crucial to pursue potential leads in the effort to comprehend this widespread neurodegenerative disorder.
“We need to do this study in humans and confirm whether the same pathway operates in the same way,” says St John.
“It’s research that has been proposed by many people, but not yet completed. What we do know is that these same bacteria are present in humans, but we haven’t worked out how they get there.”
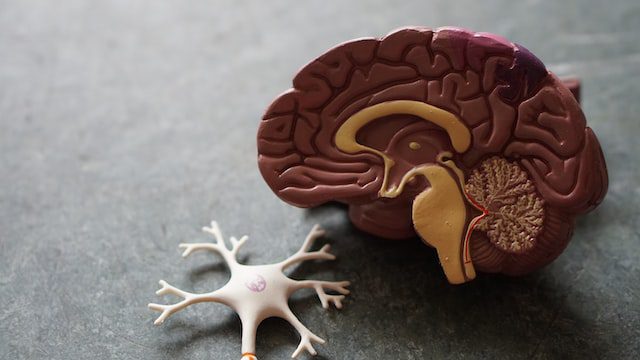
What causes dementia?
Dementia is not a specific disease. It’s an overall term that describes a group of symptoms associated with a decline in the ability to think and remember.
Causes
Dementia has many different causes, and sometimes several factors contribute. The most common cause of dementia is Alzheimer’s disease, but other conditions can lead to dementia, too.
Vascular dementia
This form of dementia occurs when blood flow to the brain is disrupted, depriving brain cells of vital oxygen and nutrients. Vascular dementia may be caused by small strokes that damage brain tissue (mini-strokes) or by more widespread narrowing and blockage of the arteries (atherosclerosis).
Lewy body dementia
In this type of dementia, abnormal structures called Lewy bodies form in nerve cells in the brain regions involved in thinking and memory (the cerebral cortex and hippocampus). Lewy body disease also can cause Parkinson’s disease-like symptoms, such as muscle rigidity and tremors. People with Lewy body disease often have visual hallucinations.
Frontotemporal lobar degeneration
This type of degenerative disorder affects the frontal lobe — the area behind your forehead — and/or temporal lobe — the region behind your ears. The lobes are involved in language, judgment, and personality.
Huntington’s disease
This is a hereditary condition that causes the progressive breakdown of nerve cells in the brain. Symptoms usually begin in middle age. Early signs and symptoms include mood changes, depression, irritability, trouble concentrating and forgetfulness. Muscle problems develop later, including involuntary jerking movements (chorea).
Parkinson’s disease
This degenerative disorder of the nervous system affects your movement. It occurs when vital nerve cells in the brain die or become impaired. Early signs and symptoms include tremors or trembling in hands, arms, legs, jaw and face; stiffness of the arms, legs and trunk; slowness of movement; and impaired balance and coordination.
Creutzfeldt-Jakob disease
This rare degenerative brain disorder is caused by an abnormal protein called a prion. Prions are found throughout your body but primarily in your nervous system tissue — particularly in your brain — where they help maintain healthy nerve cell function. Creutzfeldt-Jakob disease can occur spontaneously for unknown reasons (sporadic), be passed from one generation to another (familial) or result from exposure to contaminated human tissue during medical procedures (iatrogenic).
Normal pressure hydrocephalus
This condition occurs when too much cerebrospinal fluid (CSF) accumulates in the ventricles — cavities deep within your brain that produce CSF. The excess CSF causes the ventricles to enlarge, putting pressure on and damaging delicate brain tissue. This type of hydrocephalus is most common in older adults. It can occur as a result of injury, infection or another condition that interferes with the normal flow or absorption of CSF.
Alzheimer’s disease
Alzheimer’s disease is the most common type of dementia, accounting for 60 to 80 percent of cases. In Alzheimer’s disease, plaques and tangles form in the brain, eventually destroying nerve cells and affecting communication between them. Although current treatments can’t stop Alzheimer’s disease from progressing, they can temporarily slow the worsening of dementia symptoms and improve quality of life for people with Alzheimer’s and their caregivers.
Risk factors
There are many factors that may contribute towards a person’s risk in developing dementia. These include age, generics, injuries, among others. Let us explore each of these risks below:
Age
The risk of dementia increases with age. Most cases occur in people older than 65. However, younger adults can develop dementia, too. This is called early onset Alzheimer’s disease or early onset dementia.
Family history Having a close family member — such as a parent or grandparent — with Alzheimer’s disease slightly increases your risk of developing the condition. But the vast majority of people with a family history of Alzheimer’s don’t develop it themselves. If you have more than one first-degree relative (a parent, sibling or child) with the disease, your risk may be higher.
Genetics
In rare cases, an abnormal gene can be passed from one generation to another and cause early onset familial Alzheimer’s disease in young adults and middle-aged people. Mutations in three genes have been identified that can cause familial Early Onset Alzheimer’s: amyloid precursor protein (APP), presenilin 1 (PSEN1), and presenilin 2 (PSEN2). People who inherit one of these faulty genes will almost certainly developAlzheimer’s disease, although when symptoms begin varies widely depending on which gene is involved. These genetic mutations are responsible for less than 1 percent of Alzheimer’s cases.
Down syndrome
People with Down syndrome have an increased risk of developing Alzheimer’s disease. In fact, the majority of people with Down syndrome develop dementia by age 40.
Head injuries
Experiencing traumatic brain injury that results in a concussion or penetrating head wound may increase your risk of later developing dementia, especially if you’re older when the injury occurs. Repeated head injuries also may contribute to the development of chronic traumatic encephalopathy (CTE), a degenerative brain condition associated with memory loss, impaired judgment and depression. CTE can only be diagnosed after death through an autopsy of the brain.
Other health conditions
Conditions that damage or destroy brain cells — such as Parkinson’s disease, Huntington’s disease and Creutzfeldt-Jakob disease — can lead to dementia. Other causes include long-term alcohol abuse and infections such as meningitis or syphilis. Having diabetes or high blood pressure also increases your risk of vascular dementia.
Treatments and drugs
There’s no one-size-fits-all approach to managing dementia symptoms. The goal of treatment is to help people with dementia live as independently as possible for as long as possible. Treatment also may help relieve some of the caregiver’s burden.
Medications
A number of medications are available that can temporarily improve dementia symptoms such as memory loss, confusion and depression. These treatments don’t cure dementia or stop its progression, but they may improve quality of life for both the person with dementia and their caregivers.
Medications used to treat other conditions — such as high blood pressure, diabetes and Parkinson’s disease — also may be helpful in treating vascular dementia and Lewy body disease.
Cholinesterase inhibitors
These medications — including donepezil (Aricept), rivastigmine (Exelon) and galantamine (Razadyne) — work by boosting levels of a chemical messenger involved in memory and learning called acetylcholine. Common side effects include nausea, vomiting, diarrhea, loss of appetite, muscle cramps and fatigue. Donepezil also is available in a combination product with memantine (Namzaric). Memantine works by regulating the activity of glutamate, another chemical messenger important for memory and learning.
N-methyl-D-aspartate (NMDA) receptor antagonists
This class of medications — including memantine (Ebixa, Namenda) and dextromethorphan/quinidine (Nuedexta) — helps block the activity of glutamate, a chemical messenger that’s overactive in people with Alzheimer’s disease. Side effects can include dizziness, headache, confusion and constipation.
Antidepressants
Depression is common in people with dementia, so antidepressants may be prescribed to treat this condition. Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine (Prozac), sertraline (Zoloft) and citalopram (Celexa), are commonly used. These medications can cause side effects such as dry mouth, loss of appetite, diarrhea, nausea and weakness.
Psychotherapy
Psychotherapy or counseling may help reduce caregiver stress and improve coping skills. It also may help the person with dementia express feelings and ease anxiety or agitation.
Prevention
There’s no known way to prevent all types of dementia. However, there are a number of things you can do that may help reduce your risk. These include:
Exercise regularly
Exercise increases blood flow to your brain and reduces the risk of heart disease and diabetes, which are risk factors for vascular dementia.
Eat a healthy diet
Eating plenty of fruits, vegetables and whole grains and limiting saturated fat, trans fat, cholesterol, salt (sodium) and added sugars can help reduce your risk of cardiovascular disease — another major risk factor for vascular dementia. A Mediterranean-style diet also has been linked with a reduced risk of Alzheimer’s disease and other forms of dementia. The Mediterranean diet emphasizes fruits, vegetables, olive oil, fish and nuts while limiting red meat, processed meats, refined carbs and sweets.
Don’t smoke
Smoking damages blood vessels throughout your body by promoting the buildup of plaque in your arteries (atherosclerosis). This increases the risk of stroke and vascular dementia. Quitting smoking at any age can reduce this damage.
What is chronic nose picking
Chronic nose picking is a condition characterized by the compulsive picking of one’s nose. This behavior can lead to various problems, including bloody noses, skin irritation, and infection. In some cases, it may also interfere with a person’s ability to breathe properly.
There is no known cause of chronic nose picking, but it is often seen in people who have anxiety or obsessive-compulsive disorder (OCD). Treatment typically involves behavioral therapy and medication.
Nose picking isn’t exactly an uncommon activity. In fact, a lot of other species do it as well as up to 9 out of 10 people, according to some estimates (some a little more adept than others). Studies like this one should make us reconsider our choices even while the advantages are unclear.
Future research into the similar mechanisms in people is planned, but in the meanwhile, St John and his colleagues advise against picking your nose or removing your nose hair since it might harm the protecting tissue within your nose.
The researchers will be trying to determine if the elevated amyloid-beta protein deposits represent a normal, healthy immunological response that can be overridden.
If the increased amyloid-beta protein deposits are a normal, healthy immune response that can be reversed when the infection is fought off, that is one remaining issue the team will be trying to address.
Alzheimer’s is a remarkably complex illness, as is evident from the sheer volume of study into it and the variety of approaches scientists are using to attempt to understand it; nonetheless, each new piece of research moves us a little closer to discovering a means to stop it.
“Once you get over 65 years old, your risk factor goes right up, but we’re looking at other causes as well, because it’s not just age – it is environmental exposure as well,” says St John.
Can nose picking cause cancer?
Cancer is a disease caused by the abnormal growth of cells in the body. Although the exact cause of cancer is unknown, it is believed that certain environmental and lifestyle factors may contribute to its development. Some studies have suggested that nose picking may be a risk factor for cancer, although more research is needed to confirm this.
Nose picking is a common habit that can introduce bacteria and other foreign substances into the nose. These agents can potentially damage the delicate tissue lining the nose and lead to inflammation. Chronic inflammation has been linked to an increased risk of cancer. In addition, people who pick their noses frequently may be more likely to develop skin cancers on the face or inside the nose.
Although there is no definitive evidence that nose picking causes cancer, it is important to practice good hygiene habits to reduce your risk of infection. If you notice any changes in your skin or nasal passages, be sure to see a doctor for further evaluation.
How to stop nose picking
Nose picking is a common habit that can be hard to break. If you’re struggling to stop, there are some things you can try.
First, it is important to understand why you pick your nose. For some people, it may be a way to relieve boredom or stress. Others may do it because they have an compulsion or anxiety disorder. If you know why you’re picking your nose, you can work on addressing the underlying issue.
If boredom is the trigger, find something else to do with your hands when you get the urge to pick. This could include fidgeting with a pen or playing with putty.
If stress is the cause, find healthy ways to cope with it, such as exercise, journaling, or talking to a friend. If anxiety is at the root of your nose picking habit, talk to a therapist who can help you manage your symptoms.
In addition to addressing the underlying causes of your nose picking habit, there are some practical steps you can take to stop:
- Keep your nails short so that they can’t do much damage if you do pick.
- Apply lotion or cream around your nostrils so that picking feels less satisfying.
- Put a band-aid over your nostrils to make picking more difficult.
- Use a therapy putty or fidget toy to keep your hands busy.
- Keep a journal to track when and why you pick your nose. This can help you identify triggers so that you can avoid them.
- Talk to a therapist if anxiety is driving your nose picking habit.
If you are struggling to stop nose picking, these tips may help. By understanding the underlying causes of your habit and taking some practical steps, you can break the cycle of nose picking once and for all.







