Immunotherapy is a cutting-edge treatment option in modern medicine that utilises the patient’s own immune system to attack and eliminate infections or cancer cells. This type of treatment can come in various forms, including the revolutionary CAR T-cell therapy.
CAR T-cell therapy, also known as Chimeric Antigen Receptor T-cell therapy, involves altering the genes of a patient’s T cells to make them capable of recognisng and destroying cancer cells.
The modified T cells are then reintroduced into the patient’s bloodstream, where they can target and eliminate the cancer cells.
Currently, CAR T-cell therapies have been approved by the FDA to treat certain types of blood cancer and lymphomas, but research is still ongoing for its potential use in treating solid tumours. Other forms of immunotherapy include monoclonal antibodies, checkpoint inhibitors, and cancer vaccines.
What is Immunotherapy?
Immunotherapy is a type of treatment in which the patient’s immune system is utilised to attack any infection or any type of cancer in the body.
Depending on the type of disease there can be variety of immunotherapy options available in the modern-day cancer medicine. Immunotherapy can be either used alone or it can be given in combination with other treatment options like chemotherapy, surgery, and radiotherapy.
What is CAR T cell therapy?
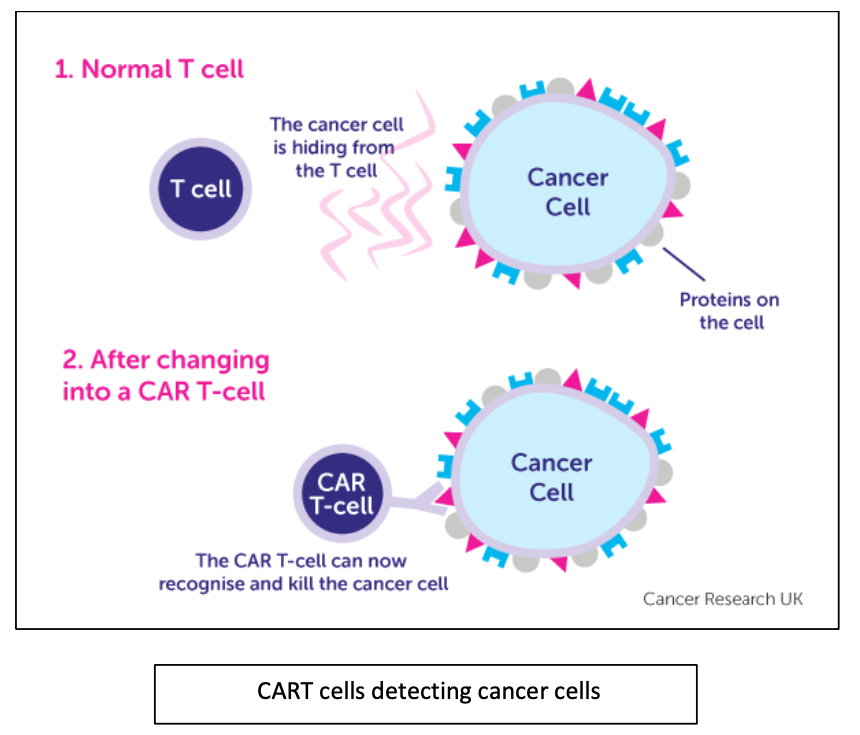
T cells (white blood cells called lymphocytes) are good at fighting infection. But it can be difficult for them to tell the difference between a cancer cell and a normal cell. So, the cancer cells can hide away and not be recognised. Scientists are trying to find ways to get T cells to recognise cancer cells. One possible way to do this might be CAR T-cell therapy.
CAR T cell therapy also known as Chimeric Antigen Receptor T-cell therapy, it is a type of immunotherapy in which a patient’s own T cells is modified (by altering the genes) to detect and kill the cancer cells.
How does CAR T-cells work?
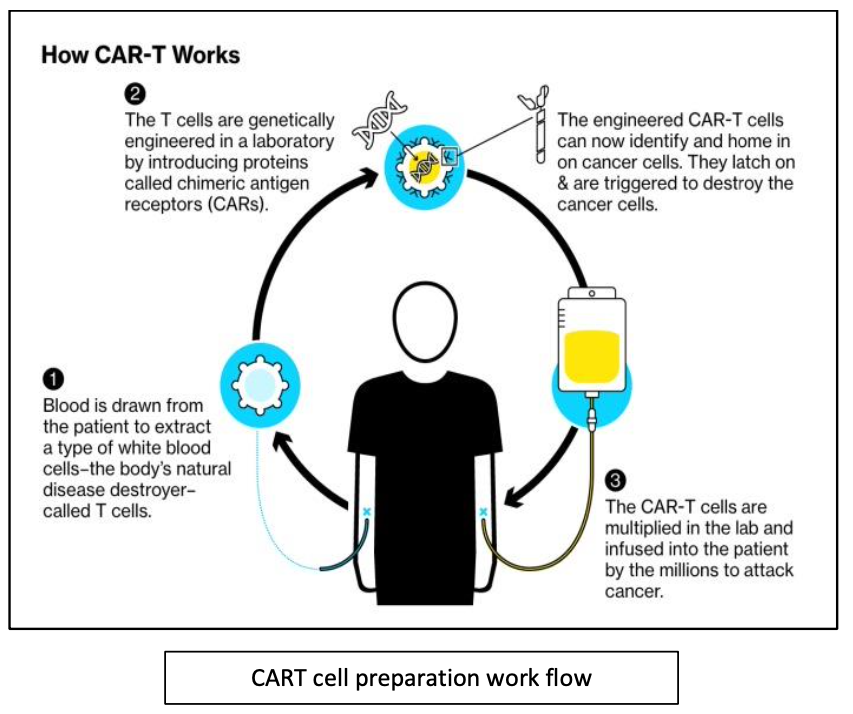
Your medical team take a sample of T cells from your blood by a process called apheresis. In lab they change these T cells and they are now called genetically engineered T-cell.
The T cell is now a CAR T-cell. These CAR T-cells are designed to recognise and target a specific protein on the cancer cells.
These changed T cells grow and multiply in the lab. Once there are enough cells you have a drip containing these cells back into your bloodstream.
The aim is for the CAR T-cells to then recognise and attack the cancer cells.
The changes they make in the lab mean that they can stay in your body for long periods of time, recognising and attacking the specific cancer cells. Researchers are still looking into how long they might stay in the body.
Disease conditions treated:
CAR T-cell therapies are approved by the US Food and Drug Administration (FDA) to treat some kinds of lymphomas and leukemias, as well as multiple myeloma (types of blood cancer). CAR T-cell therapy is typically used after other types of treatment have been tried. There has not been an enough success with CARTs for solid tumors and research is still in progress for its development.
Examples of CAR T-cell therapies currently approved include:
- Tisagenlecleucel, also known as tisa-cel (Kymriah)
- Axicabtagene ciloleucel, also known as axi-cel (Yescarta)
- Brexucabtagene autoleucel, also known as brexu-cel (Tecartus)
- Lisocabtagene maraleucel, also known as liso-cel (Breyanzi)
- Idecabtagene vicleucel, also known as ide-cel (Abecma)
- Ciltacabtegene autoleucel, also known as cilta-cel (Carvykti)
There are other types of immunotherapies:
Monoclonal antibodies
Antibodies are produced by B cells in the body which helps in fighting the infection and cancer. Monoclonal antibodies are produced in the lab which mimic the natural antibodies found in body. These are called monoclonal because they are of same clone I.e., they are generated in such a way that they can target any one type of protein molecule found on the cancer cells or immune cells.
Checkpoint Inhibitors
T cells have checkpoint proteins that can either turn it on or off for their immune response. When there is an infection the T cells express checkpoint protein for the immune response but it is for certain period till there is an infection once the immune response is not required then there are other checkpoint proteins that turn it off for the immune response.
Some cancer cells itself express checkpoint proteins which disable T-cells from attacking them, thus checkpoint inhibitors help to block such proteins either on T cells or on cancer cells to provide a good immune response against the cancer cells.
Vaccines to treat cancer
Researchers are looking at whether vaccines can help the immune system to recognise and attack cancer cells. In the same way that vaccines work against diseases, the vaccines are made to recognise proteins that are on cancer cells. This helps the immune system to recognise and mount an attack against those cancer cells.
Cytokines
Cytokines are a group of proteins in the body that play an important part in boosting the immune system. Interferon and interleukin are types of cytokines found in the body. Scientists have developed man made versions of these to treat cancer.
Conclusion
CART cell immunotherapy has been a remarkably successful treatment plan for patients who has been terminally ill but as with other cancer therapies it comes with certain side effects however it has shown over 30 to 40 percent success rate, these data are from treatment of patients with liquid cancers.
For solid tumours, the CAR T-cell clinical trials are still in the initial phase and require more development of it. As other type of immunotherapies is also available, it totally depends on the type of cancer and the stage of the disease that what type of treatment will best suit to the patient and give a good clinical response.